The chance of complications with a newly created urinary diversion is rare, but they can still arise. In this article, we will talk about the most common complications that might occur after urostomy surgery.
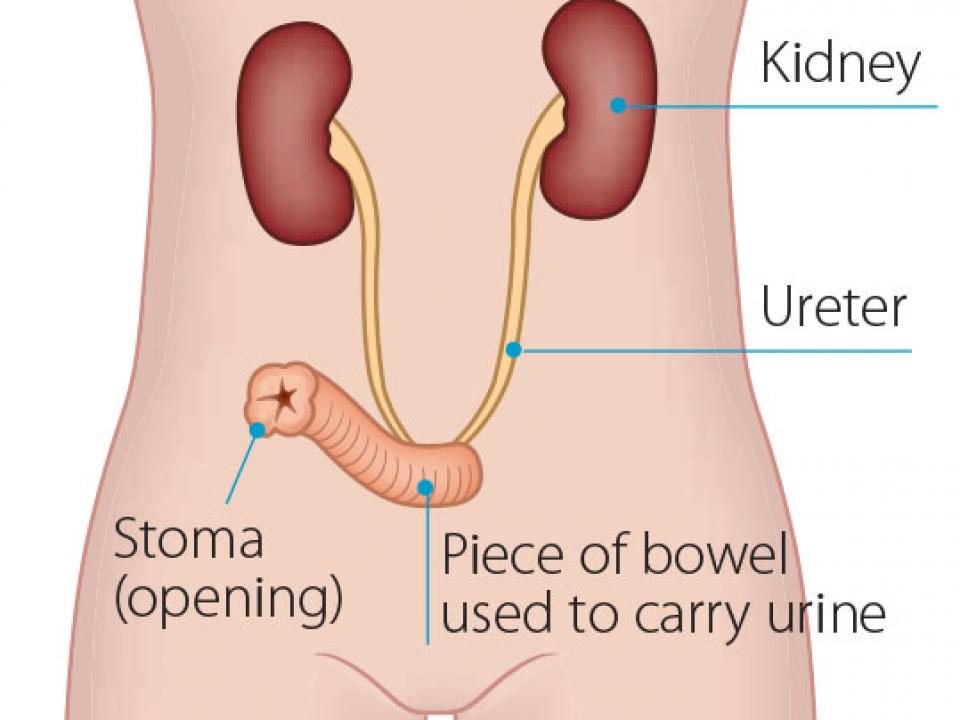
What is a urostomy?
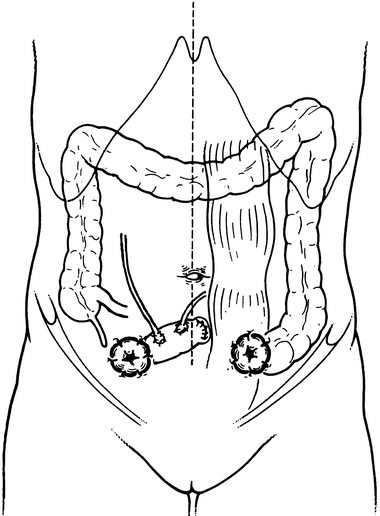
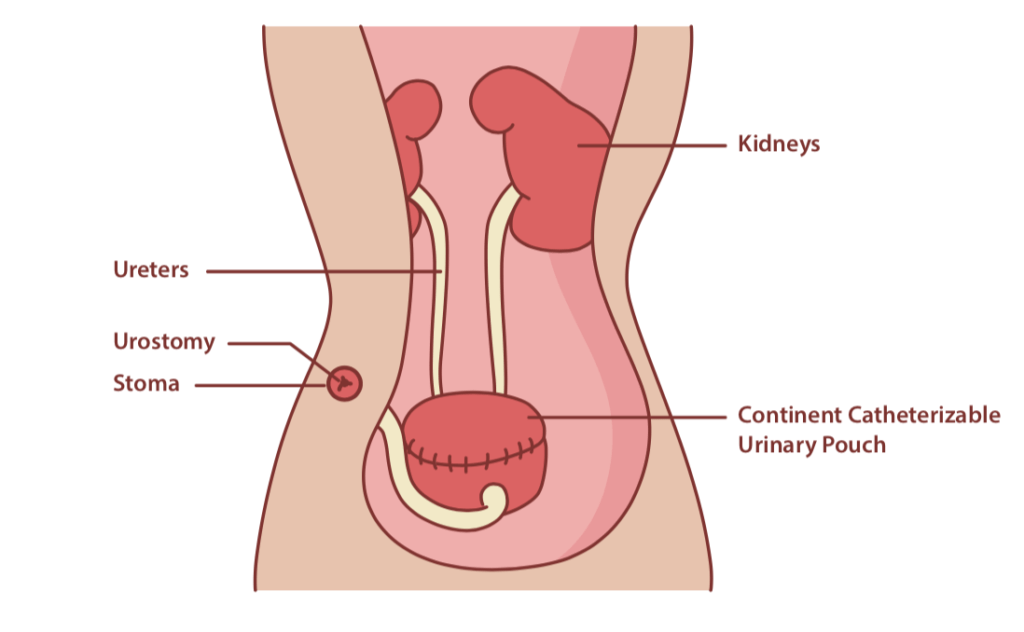
The creation of an opening in the belly to allow urine to pass out after removal of the bladder is known as urostomy surgery. To create this opening, the surgeon resects a piece of the small intestine. It is usually 6 inches long. One end of that piece is sewn. The surgeon attaches the ureters to that end. The other end appears on the belly, creating the stoma.
Urinary diversion surgery
An alternative to a urostomy is the continent pouch, which involves the creation of an internal pouch that stores urine. This pouch has a valve that passes urine either to the outside of the body through the abdominal wall, or to the urethra, activating the natural urinary pathway again. With a continent pouch, you are not going to have to wear an ostomy pouch on your belly. Instead, you will need to insert a catheter into the opening in the belly to remove urine from the internal pouch. Types of continent pouches include an Indiana pouch and a Kock pouch.
What to expect after surgery
You will need to stay in the hospital after surgery for 5-7 days. This hospital stay is crucial because there is a risk of blood clotting in the surgery site. This blood clotting can cause severe complications, which might even be life-threatening.
After surgery, you may have swelling in your genitals, and there might be some discharge from the urethra. You may also experience constipation, diarrhea, soreness, and pain. All these are normal.
You may shower three days after surgery, but make sure to avoid using soap. Clean your incision with water. If the incision turns redder or drains pus, contact your doctor immediately.
Urostomy complications
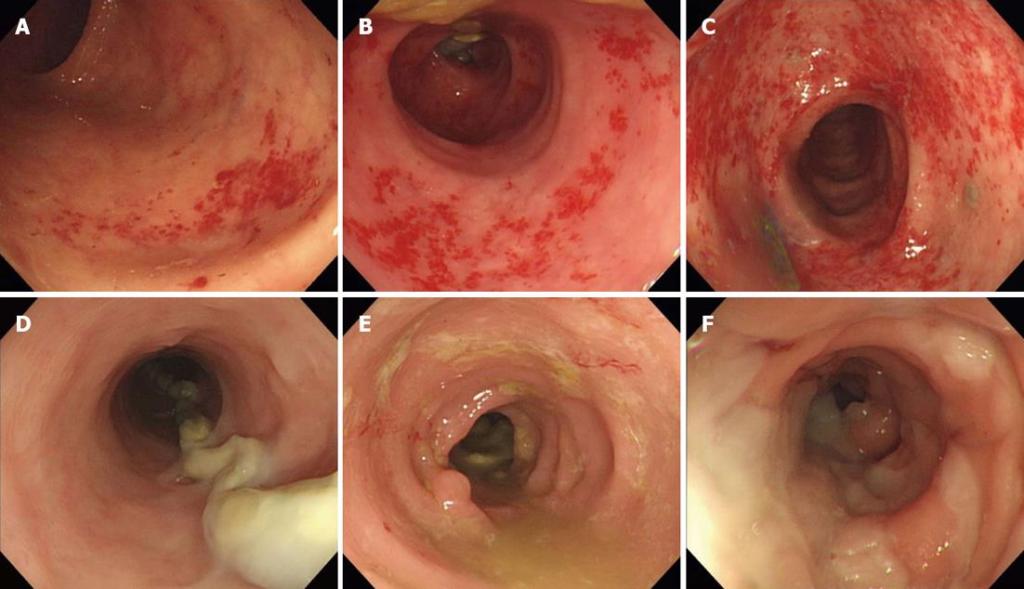
Here is a list of a few complications that might arise with a continent pouch. These complications are not quite worrisome and subside over time.
- You may experience some leakage of urine. It is because the internal pouch is not big enough to hold a large volume of urine. Over time, it will get bigger, and the issue of leakage will settle.
- The opening in your belly may discharge thick mucus. Because the opening is made of the intestine, its living tissues still generate mucus.
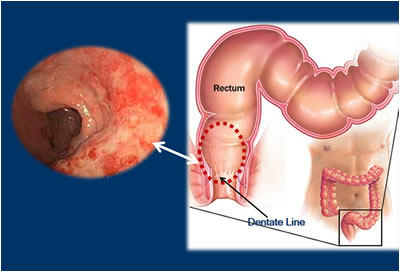
- There may be some swelling in the stoma after surgery, but its size will reduce over time.
Some issues can be worrisome.
- The urine turning light pink is the sign of bleeding. It is generally due to the irritation caused by the catheter. The body will adapt to catheterization over time, and the bleeding will settle. However, you may have to contact your doctor immediately if the bleeding is heavy.
- You will need to contact your healthcare provider if the urine is dark, cloudy, and foul-smelling.
- Watch out for bulging and pain in the abdomen.
- Contact your doctor immediately if the stoma becomes dry, protrudes, sinks, or changes shape.
Most of these issues should subside over time, but you have to have the right information to prevent these common complications from getting out of control.